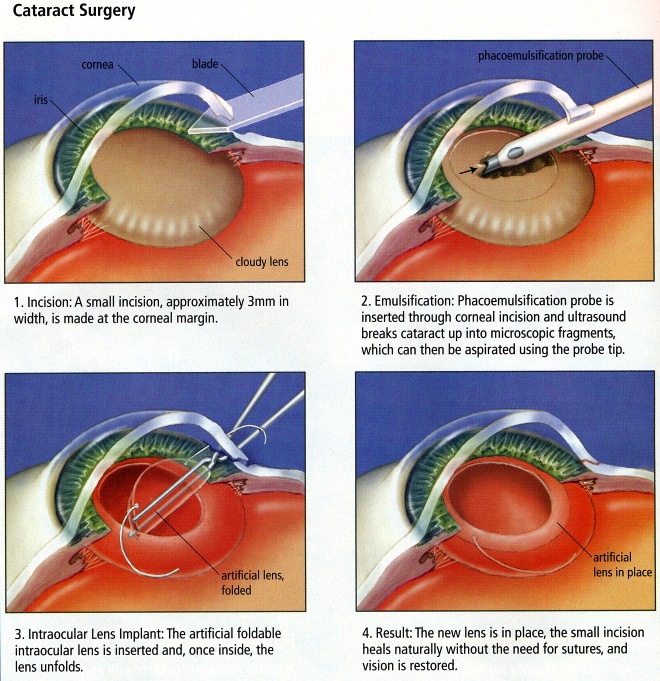
Cataract Surgery often takes between 10-15 minutes and is an outpatient procedure, which means there is no overnight stay, no heavy anaesthesia and very little down time. Our surgeons use the latest technologies to determine what your precise eye care needs are; and offer an array of implant options for all patients and lifestyles.
CATARACT CARE
With age, our bodies change. Visual impairment often occurs in the later stages of our lives. One of the main causes is cataracts, but for this particular problem there are solutions.
Cataracts cloud the normally clear lens of the eye, leading to blurred or misty vision. They typically occur in the sixth and seventh decades of life, slowly and subtly stealing a patient’s vision. Sensitivity to glare, visual distortions, and difficulty in distinguishing colours may indicate that a cataract is developing.
There is no real way to avoid developing a cataract. Your general health, your genes, and diseases such as diabetes can contribute to the development of early cataracts.
STATE-OF-THE-ART TECHNOLOGY
We also pride ourselves on being able to provide premium technology to correct visual impairment and achieve the best results. If you qualify for cataract surgery you can rest assured that our equipment and instruments are of the highest standard.
Our clinic is a refractive practice. Our staff are highly qualified and trained, and constantly applying new, improved techniques.
We apply tried and tested evaluation and assessment techniques, and have an individualized approach to each patient.
PATIENT-CENTERED
We take cataract surgery very seriously and care for each patient’s vision as if it were our own.
We’re very patient-centered at the Jaibo Eye hospital. We listen to our patients and do what they want. If a patient wants regular cataract surgery then we provide it.
At the Jaibo Eye hospital you can rest assured that we treat every patient like a member of the family. The other thing that sets us apart is the combination of our empathy with patients and our clinical acumen. We guarantee sensitive care, and our patient feedback suggests high satisfaction rates.
On arrival you will be asked to fill in a registration card. Please give your complete permanent address with telephone number. You will be asked to take a seat until our receptionist accompanies you to your vision test..

CAUSES
The causes of corneal diseases are varied, as too are the individual diseases or disorders themselves. Thus, there are no common causes.
However, some of the risk factors associated with corneal diseases are hereditary, that is, a genetic condition passed down by your parents may be the cause. Trauma and infections can also be a precursor to corneal diseases.
Secondary causes include:
- Other eye diseases that may affect the cornea
- Autoimmune diseases
- Growths
- Tumors
THE MOST COMMON CORNEAL DISEASES
There are several different types of corneal disease. The most commonly seen are:
Keratitis
An inflammation that affects the cornea. The inflammation occurs as a result of an infection, a fungus, or some bacteria entering the cornea.
Ocular herpes
There is no real way to avoid developing a cataract. Your general health, your genes, and diseases such as diabetes can contribute to the development of early cataracts.
Shingles (herpes zoster)
Shingles is a condition whereby the Chicken Pox virus reappears in people who have already had Chicken Pox, this mostly happens in later life. Like ocular herpes, shingles can cause sores on the cornea and the condition is controlled with anti-viral treatments.
Keratoconus
A condition in which the cornea undergoes a distortion of the curvature and thins. This condition may also cause a loss of vision and/or near-sightedness.
Corneal dystrophies
Corneal dystrophies are a grouping of diseases that cause problems in the corneal structure.
Dry eyes is the most common ailment that the doctors at Jaibo Eye hospital encounter on a daily basis. The right dry eye treatment can only be prescribed after a dry eye specialist has properly diagnosed the type and severity of the disease

WHAT ARE THE DRY EYES SYMPTOMS?
Another common dry eye symptom includes eyes that water constantly. This often confuses patients as they don’t realize that this relates to dry eyes. These tears, known as reflex tears, are different from the normal tears (basal tears). They do not have the right composition of the oil and water components that are required for the eye to stay healthy and lubricated. The purpose of reflex tears is simply to flood the eye as a response to an irritant in the eye, trying to flush it out.
The typical dry eyes symptoms include:
- Eye fatigue
- Irritable, scratchy eyes
- Lack of visual clarity
- Light sensitivity
- Redness or discomfort
- Stringy eye mucus discharge
WHAT ARE THE AVAILABLE DRY EYES TREATMENTS?
The good news: There is an FDA-approved treatment to manage the chronic disease well. At Jaibo Eye hospital , the first line of dry eyes treatment is always to prescribe over the counter drops or prescription drops to try and manage the disease. If this dry eye medication doesn’t work and the disease persists, the doctor may recommend tear plugs (punctual plugs) or Lipiflow.
Drops:
Doctors recommend Lubricating and steroid drops commonly for dry eyes treatment.
Punctal Plugs:
These plugs are inserted into the tear duct to prevent the tears draining from the eye. This helps the eye to lubricate itself.
Lipiflow:
This is the only FDA-approved procedure for dry eyes. A device applies heat to the lower lids and the upper globe, while protecting the eyes themselves from direct heat. Pulsating squeezes are applied to massage the eyes and release the blocked glands.
Glaucoma treatment is only applicable when vision loss has not occurred.
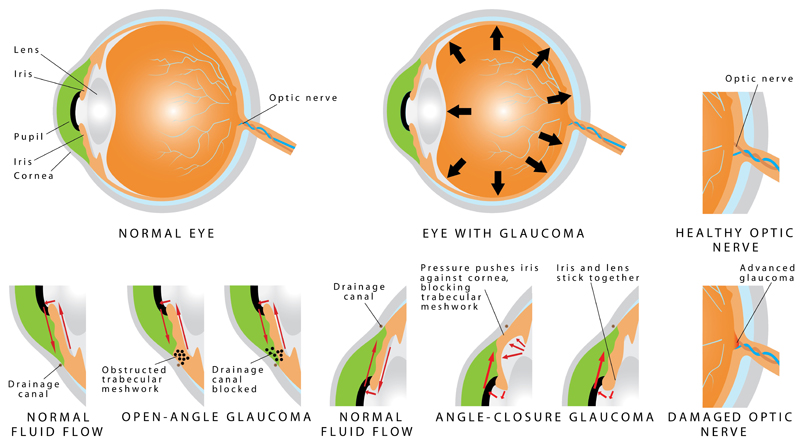
WHAT CAUSES GLAUCOMA?
A sustained fluid pressure on the optic nerve of the eyes causes glaucoma. In healthy eyes, the fluid (aqueous humor) flows through a mesh-like ‘channel’. The blockage of this channel causes glaucoma. The blockage itself may be caused due to a number of reasons like:
Blockage of blood vessels in the eye
- Inflammation
- Inheriting the disease from a parent
- Chemical injury to the eye
- Physical injury to the eye
- Severe infection
DEPENDING ON THE BLOCKAGE TYPE, GLAUCOMA CAN BE CATEGORIZED AS ONE OF THE TWO:
Open-angle glaucoma
Known as ‘wide-angle glaucoma’, this is the most common type of the two. In this case, the channel clogs over time which causes the increased pressure, while its drainage angle (where the cornea and iris meet) is normal.
Close angle glaucoma
Known as ‘angle-closure glaucoma’ or ‘narrow-angle glaucoma’, this type occurs when the iris narrows the drainage angle by bulging forward. The pressure is built suddenly when the pupil dilates (e.g., in a dark room) and blocks off most or all of the fluid drainage. This is known as a ‘glaucoma attack’. Ophthalmologists treat these cases as an emergency.
DEPENDING ON THE BLOCKAGE TYPE, GLAUCOMA CAN BE CATEGORIZED AS ONE OF THE TWO:
Depending on the severity of glaucoma, it can be treated in various ways. Typically, eye specialists prescribe drops or pills as open angle glaucoma treatment, but when the medication doesn’t work or the eye does not tolerate it, they recommend a glaucoma surgery.
There are two types of surgeries for treating glaucoma:
1. LASER SURGERY
Eye specialists recommend this glaucoma treatment when damage occurs to the optic nerve and/or when the pressure is critically high. In glaucoma laser surgery, a focused beam of light is used to create small openings in the eye tissue, allowing the aqueous humor to circulate easily. Examples of this type of surgery include:
- Argon Laser Trabeculoplasty (ALT): This involves an argon laser beam opening the fluid channels of the eye, easing the drainage. This method lowers the risk of increased pressure post-surgery. Doctors typically prescribe ALT for patients with open angle glaucoma.
- YAG Laser Peripheral Iridotomy (LPI): Ophthalmologists often recommend this procedure for patients with closed angle glaucoma. This surgery makes a small hole in the iris to increase the drainage angle back to the normal level.
How long does a laser surgery take? Is it painful?
A laser surgery takes about 5-10 minutes, and is completely painless. However, there may be a light stinging sensation.
What is the recovery time for laser surgery?
The recovery time for this surgery is quite short. You can go home right after your surgery. Your vision may become a bit blurred, but it will go away in a day or two. Doctors suggest follow ups depending on individual case types.
What are the precautions and postoperative care for laser surgery?
The success rate of laser is quite high (75% for ALT) but not as high as that for trabeculectomy.
- Do not rub your eye(s)
- Do not wear eye makeup for at least a week after surgery
- Take any prescribed medication religiously
- Wash your hands before using eye drops
- Wear sunglasses to protect your eyes
If your eye becomes red or starts to irritate, seek professional help immediately.
2. INCISIONAL SURGERY
When the laser surgery does not work, eye specialists may recommend trabeculectomy. Small incisions are made in this glaucoma treatment to create new channels for fluid drainage.
How long does an incisional surgery take? Is it painful?
This type of surgery can take about 20-30 minutes. It isn’t painful, either, because the eye is anaesthetized during the surgery.
What is the recovery time for trabeculectomy?
The recovery time for this surgery is higher than laser. Your doctor might recommend you several eye drops to prevent infection and reduce inflammation. This can take a few months.
What is the success rate for trabeculectomy?
The success rate of trabeculectomy at five years is 80%.
What are the precautions and postoperative care for trabeculectomy?
- Always wash your hands before using the eye drops, and avoid touching the tip to your eye
- Avoid bending over or lifting heavy objects
- Avoid strenuous physical activities
- Do not use eye makeup like eye pencil or kohl
- Protect the eye from external injury
- Use medication as recommended by your doctor
- Wear UV sunglasses during the day
WHO IS AT RISK?
Dry eyes is common in all demographics. It is especially common in the elderly, females with light eyes, people who wear contact lenses, teenagers who spend a huge amount of time on screens and smokers. It is also common in people with existing ailments like arthritis, Sjögren’s syndrome or any other immune disease.
Being on a computer for long periods of time without taking breaks is a major contributor to dry eyes. People who do this blink about 60% less than they would normally, which decreases the chance of their.

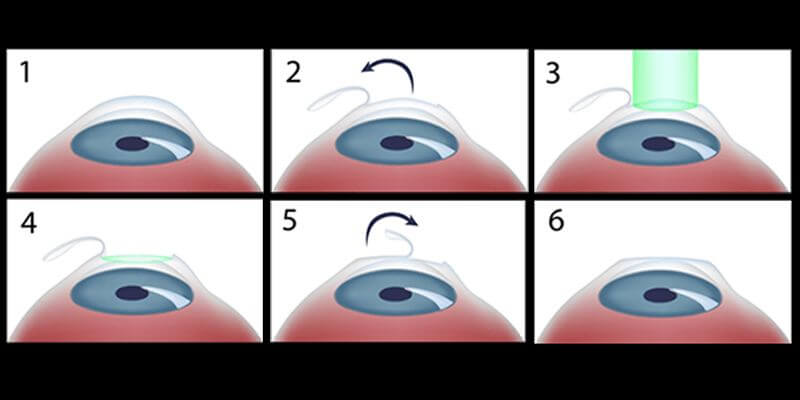
Lasik Surgery
There are many choices for people who have vision needs, and LASIK surgery is only one of them. Nearsightedness and farsightedness are common. As much as 60 percent of the population have needed glasses or contacts at some point in their lives. However, some people find it difficult to deal with vision aids. They want to find out about more permanent solutions. For these people, LASIK surgery may be a good choice.
WHAT IS LASIK SURGERY?
LASIK surgery is most often a permanent cure surgery that restores your vision. It is not a cosmetic procedure and will not affect the way your eyes look. Depending on your age when you get it, you can expect to enjoy years or even decades of near-perfect vision. However, as you age, you may eventually need vision aids again.
As time passes, we all develop a need for reading glasses, which is not related to whether you have had LASIK or not. Rather, It’s Mother Nature saying you are losing your near vision after 40.
WHAT DOES LASIK STAND FOR?
LASIK stands for laser-assisted in situ keratomileusis. This term can essentially be translated as “reshaping of the cornea in its place with lasers.” It is a kind of refractive surgery. This manually corrects the shape and positioning of the cornea with the use of lasers. It is the most common type of ophthalmic surgery. LASIK can be a good fit for those who are nearsighted, farsighted, and those who have astigmatisms.
During a LASIK procedure, an eye doctor uses lasers to reshape your cornea. This lets light enter through the eye on a proper path. When light is directed correctly toward the retina, you will be able to see more clearly.
LASIK was once a groundbreaking surgery. Now, it is a simple in-and-out procedure. It is performed thousands of times a day in ophthalmic offices all over the country.
WHO IS A GOOD CANDIDATE FOR LASIK SURGERY?
LASIK has helped hundreds of thousands of patients improve their vision. But not everyone is a good candidate for the procedure. There are a few things that are required for you to qualify for LASIK surgery.
LASIK has an overwhelmingly high success rate. However, anyone who is considering it should know that there are minor risks involved. Occasionally, a LASIK procedure results in vision that is not perfect 20/20. As with any surgical procedure, there is a chance of complications. The ideal candidate for LASIK should be able to accept the possibility of a poor outcome. Most people who go through LASIK surgery experience improved vision with no complications.
The LASIK procedure is quick — around 8-15 minutes — if performed by our experts’ doctors and most people can return to work the next day.
To qualify for LASIK, your prescription must also remain unchanged for a minimum of two years. For this reason, it is recommended that people wait until after 18 years old before having LASIK surgery. Before this point, your eyes are still developing, and your prescription is likely to get worse every year or two. LASIK is not a good idea then, since the procedure needs to be repeated as your eyes continue to develop.
You may be a good candidate for LASIK, if you are willing to undergo surgery. Also, if you have had a stable prescription for two years or more, and are in generally good health. If you have glaucoma, cataracts, or another eye disease, you should not get surgery.
HOW DO YOU PREPARE FOR LASIK SURGERY?
Your eye doctor can help prepare you for your LASIK surgery. However, there are a few things that you should know.
A day or two before your surgery, avoid wearing any eye makeup. You should also not use creams, liniments, or other products on or around your eyes. You may also be asked to wash your face, specifically your eye area, before coming in for your procedure. This is to ensure that there is no dirt or debris around the surgical site.
You will also need to take some time off from work. Although LASIK is a quick procedure, your eyes will take a few days to be back to full capacity.
When you are getting ready to go in for your surgery, do not wear any accessories or jewelry. This could get in the way of the lasers that are used during the procedure. Dress simply and comfortably.
You should also make plans to get a ride to and from your surgery. Your vision will not be ready for the road for a few days, so you should not drive.
Before your surgery, you will most likely be able to eat and take medications as usual. However, you should confirm these details with your doctor before the procedure.
WHAT HAPPENS DURING YOUR LASIK SURGERY?
LASIK surgery is an extremely quick procedure. It is entirely possible that you will be in and out of the operating room within 15 minutes. It is also not painful, so you will not be given any drugs. However, you will receive a local anaesthetic in the form of simple eye drops. These will keep you from feeling any pain during the procedure. If you are feeling nervous, ask your doctor if they would be willing to give you a mild sedative. This will help you relax in the operating chair.
Although the surgery is painless, you will be awake for it. Most people find that this is not as nerve-wracking as they expected. Once your LASIK surgery is done, you should go home and rest. When your eyes heal, you will be able to enjoy 20/20 vision once again.
Our eye specialists at The Jaibo Eye hospital
MACULAR DEGENERATION
One of the most common retina disorders is macular degeneration. The condition slowly destroys your central vision, making it difficult to read or recognize faces.
“Age-related macular degeneration” is a disease that tends to affect people over 50. The retina tends to grow thinner as we age.
Sight loss is usually gradual, but in rarer cases it can be much quicker. However, your peripheral vision remains, meaning that you do not go completely blind.
At Jaibo Eye hospital our treatments aim to help patients make the most of their remaining vision. For example, magnifying lenses make reading easier. As with most diseases, early diagnosis of macular degeneration can help patients better adapt and cope.
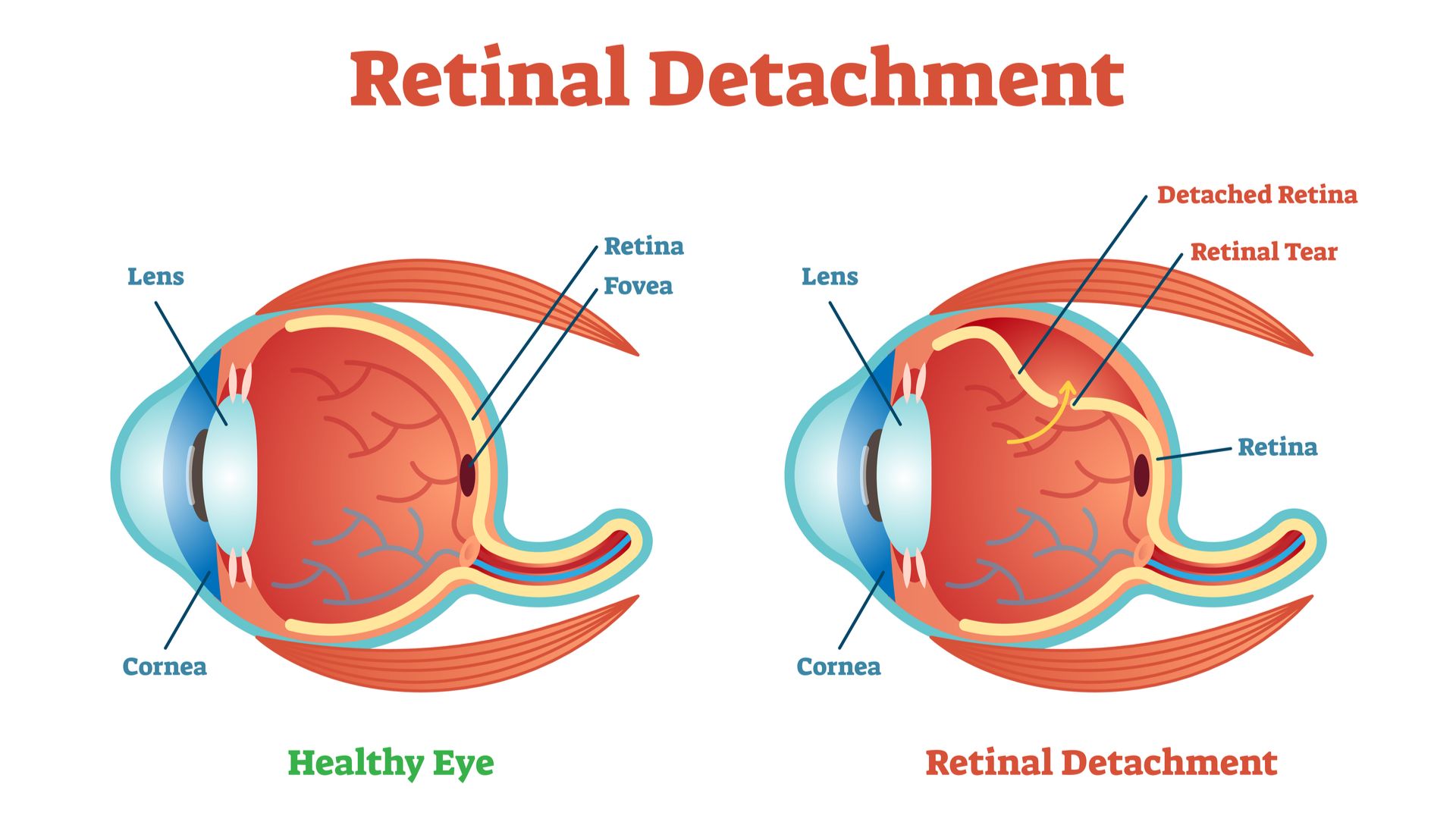
RETINA DISORDERS – TEARS AND DETACHMENTS
Retinal tears occur when part of the retina pulls out of its normal position. Symptoms indicating this might be happening can include the sudden appearance of flashes. At the same time, any floaters (roving specks) in the eye may suddenly increase in size or number. Other symptoms include seeing a shadow at the periphery of your vision, or a sudden reduction of vision. Blurred vision and seeing a curtain-like shadow moving across your field of vision are also possible symptoms.
It’s important to act upon such symptoms quickly to minimize the risk of permanent vision loss. You may be at greater risk if you are extremely near-sighted or you have a family history of retinal detachments.
Causes of retinal detachment include injury, diabetes or the leaking of gel-like material (vitreous) through a retinal tear.
DIABETIC RETINOPATHY
Jaibo Eye hospital also treats diabetic retinopathy, which causes damage to the retina’s blood vessels. If you have diabetes, you have a good chance of having diabetic retinopathy.
Symptoms include blurred vision, the appearance of floaters, difficulty with color perception, and eye pain.
Diabetes causes elevated sugar levels, and this can damage the small blood vessels feeding the retina. Diabetic macular edema occurs when damaged blood vessels leak fluid into the retina, causing a swelling in the center of the eye.
The longer you have had diabetes the more at risk of diabetic retinopathy you are. Other risk factors are high blood pressure and cholesterol levels.
To test for diabetic retinopathy the specialist normally puts drops in the eyes to make them open wide. This allows a better view of the retina.
UVEITIS
Uveitis covers many eye problems but broadly speaking it is a kind of eye inflammation. It affects part of the eye wall (uvea). Uveitis can cause swellings that damage or destroy eye tissues. Symptoms can appear suddenly and include redness of the eye, pain and blurred vision. People aged 20-50 are most likely to be affected.
Autoimmune disease, infection, or injury appear to be the main causes. The condition can lead to permanent vision loss, so early diagnosis and treatment are vital.
The uvea lies between the white part of your eye – the sclera – and the inner layers of your eye.
The uvea contains the iris, the ciliary body (helps the eye focus) and the choroid (blood vessels that bring nutrients to the retina).
RETINAL VASCULITIS
Retinal vasculitis causes blurred vision, floaters and decreased the perception of colors. Vascular branches of the retinal artery become inflamed.
Temporal arteritis is a blood vessel inflammation that may lead to blurred vision. In some cases, it can block the artery to the eye resulting in blindness. It is most common in those aged over 70. Treatment options include high doses of steroids.
If you have any concerns or questions relating to retina disorders please contact The Jaibo Eye hospital . Our Specialist will discuss with you and recommend the best appropriate treatment for you.
Neuro-Ophthalmology is a super specialty that merges the fields of neurology and ophthalmology. Neuro-ophthalmologists are responsible for the diagnosis and management of complex systemic diseases of the nervous system that affect vision, eye movements and alignment, as well as pupillary reflexes.
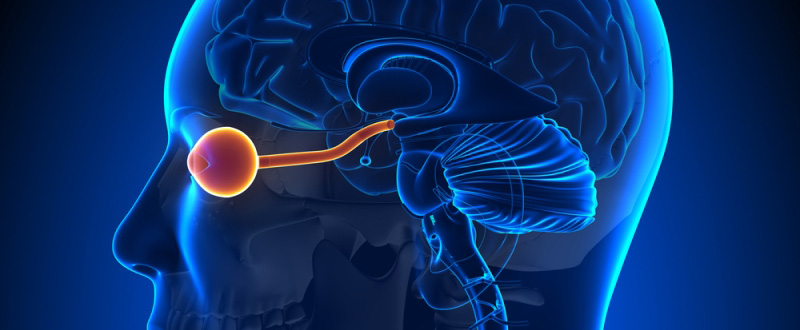
When should you visit your Neuro-Ophthalmologist?
Your eye doctor will usually suggest you visit an expert in Neuro-Ophthalmology after a comprehensive eye examination, in case you need special care. Often, the symptoms that prompt such a referral include those associated with optic nerve disease or diseases of the visual pathway (the nervous system component that connects the eyes to the brain). Other reasons could be the diseases affecting the pupils of the eye, and certain kinds of squint (especially paralytic).
Common Symptoms that Require Attention
The typical symptoms that could signify a neuro-ophthalmological problem include:
- Sudden decrease or loss of vision
- Sudden transient loss of vision (called transient ischemic attack or eye stroke)
- Visual hallucinations
- Double vision or diplopia
- Intractable headaches
- Pupillary abnormalities (sluggish reaction, the difference in size of the pupils)
- Sudden onset of difficulties in identifying colours
- Inability to tolerate bright light
- Visual Field Defects
- Squint or strabismus (especially adult onset)
Types of Eye Diseases treated by a Neuro-Ophthalmologist
The common eye diseases that require attention from a neuro-ophthalmologist include:
Optic Neuritis
It is a condition which presents as a sudden onset loss or decrease in vision due to inflammation of the optic nerve. It can be due to an infection, or an autoimmune response. Optic neuritis is often associated with Multiple Sclerosis(MS).
Papilledema
Papilledema is characterized by the swelling of the optic nerve head (the part of the optic nerve which can directly be seen by your eye doctor during a retinal evaluation) due to increased pressure from inside the brain. It may be due to tumors, infections like meningitis, encephalitis, etc.
Toxic or Nutritional Optic Neuropathy
The optic nerve may be damaged due to toxic substances found in tobacco & alcohol. In fact, the optic nerve damage is often due to lack of nutrients and deficiency of vitamin B-complex and folic acid as well. These diseases also present as decreased vision.
Squint or Strabismus
A misalignment of the eye, especially when sudden in onset, and associated with double vision is often due to paralysis of one or more of the small muscles of the eye, and is called paralytic strabismus. The eye shows limitations of ocular movement as well.
Common Tests for Diagnosis and Management of Neuro-Ophthalmology Diseases
Retinal vasculitis causes blurred vision, floaters and decreased the perception of colors. Vascular branches of the retinal artery become inflamed.
A comprehensive eye examination is always the mainstay of the disease diagnosis. In addition to this, your doctor will also advise one or more of these special tests to conclude to plan your treatment. These tests include:
- Orthoptic evaluation
- Evaluation of ocular movements
- Diplopia charting
- Neurological visual fields screening
- Optical coherence tomography of the optic nerve head
- Evaluation of contrast sensitivity and color vision
- Imaging studies including CT scan, MRI and MR venogram
- Lumbar puncture

Children are not miniature adults. Their eyes, visual needs, and disorders are entirely different than from those of adults. Since they are rapidly growing, and are yet to develop a fully mature eye-brain coordination, disorders of vision in children require special attention and focus. This is why pediatric ophthalmology has evolved as a specialized discipline, and indeed a subspecialty in ophthalmology.
The pediatric ophthalmologist is responsible for taking care of the visual attention needs of the children, and ensuring a proper visual development regarding both function and structure (including cosmesis).
How is the eye of the child different?
Just as a particular doctor is required for your child’s general health, even the eyes of a child need specialist care. It is because the considerations in terms of eye care are entirely different from those in adults. The reasons for this are as follows:
- The brain-eye connections are not fully made, so any deprivation of vision in early childhood, if it remains uncorrected, can result in lazy eye or amblyopia. These means that the visual potential of the child becomes limited, and even proper corrective glasses cannot help in later help. Amblyopia therapy is critical in the early years of life
- The congenital anomalies or disorders of development show up in the early years of life. These can range for refractive errors which merely require corrective glasses, to squint or misalignment of eyes, congenital nasolacrimal duct block, ptosis or lid droop and even cataract and glaucoma.
- Infants who are born premature, of low birth weight or who have a prolonged tumultuous stay in the newborn nursery, are at risk for a disease called Retinopathy of Prematurity, RoP. RoP is potentially vision threatening and must be screened for in these high-risk
- In settings of malnutrition, children are susceptible to Vitamin A deficiency, and its attendant eye problems including dry eye, corneal ulcers, and even blindness. Fussy and choosy eaters may also sometimes be deficient in some micronutrients despite being healthy and well fed otherwise.
- Children, because of their active lifestyle and playing outdoors are more prone to eye allergies and trauma.
- TV viewing, increased screen time and video games have given rise to a particular set of concerns in this age group.
- There is a set of eye tumors and malignancies that are typical of infancy and childhood like retinoblastoma.
What are the symptoms and signs of eye problems in children?
- Reading disability and problem in school in copying what is written on the board could be an indication of poor vision
- Any squint or misalignment of the eyes
- Any frequent headaches, eye rubbing, red eye, recurrent eye infections and watering from eyes
- Any family history of eye disorders including the need for glasses (refractive errors), can be passed from one generation to another and must be evaluated early on in life. The frequency and schedule of an eye examination in children are mentioned here.
Which is best hospital for eye care in children?
For your child’s eye care, Jaibo Eye hospital is the best eye clinic and some of the top pediatric ophthalmologists in Gwalior , who understand the importance of healthy eyes and good sight for the overall development of a child.
The environment in the pediatric ophthalmology department is always relaxed, and the staff always eager to play with the children, ensuring trouble and hassle-free eye check-up for your precious little one.
This, of course, comes with the Jaibo Eye hospital promise of professional integrity, and state of the art technology, at affordable rates for all, at a center near you.
What are the special tests and services that JAIBO Eye Centre offers for children?
The eye specialists and the ancillary team at Eye Centre are fully aware that our children require special nurturing and care to thrive, and achieve their full potential. The team of eye care professionals is happy to partner with you in your efforts to ensure the best eye care for your child.
JAIBO Eye Centre offers state-of-the-art technology in child vision care, with the empathy and compassion that is the hallmark of the patient acre with the group. The specialist services and eye tests for children, in addition to primary eye care, include:
- Vision assessment and refraction under dilation
- Squint assessment and evaluation of binocular vision
- Amblyopia therapy
- Synaptophore assisted eye exercises for stimulating the eye muscles and binocular vision.
- Management of all childhood infections and allergies
- Examination under sedation or anesthesia, if indicated. Comprehensive pre-anesthetic check-up and post-operative care.
- Glasses and low vision aids
- Surgical and medical management of childhood and congenital disorders, as indicated: congenital cataract, congenital ptosis, glaucoma and squint.
The surgeries performed routinely by the pediatric eye surgeons at JAIBO Eye Centres include:
- Phacoemulsification with intraocular lens implantation with and without posterior capsulorhexis and vitrectomy
- Intraocular lasers for RoP
- Ptosis surgeries including sling surgery and other lid reconstructions
- Complex and straightforward squint surgeries including recti and oblique muscles, syringing and probing, dacryocystorhinostomy, trabeculectomy with MMC and Ahmed Glaucoma Valve implantation, as well as complex vitreoretinal surgeries and retinal lasers.
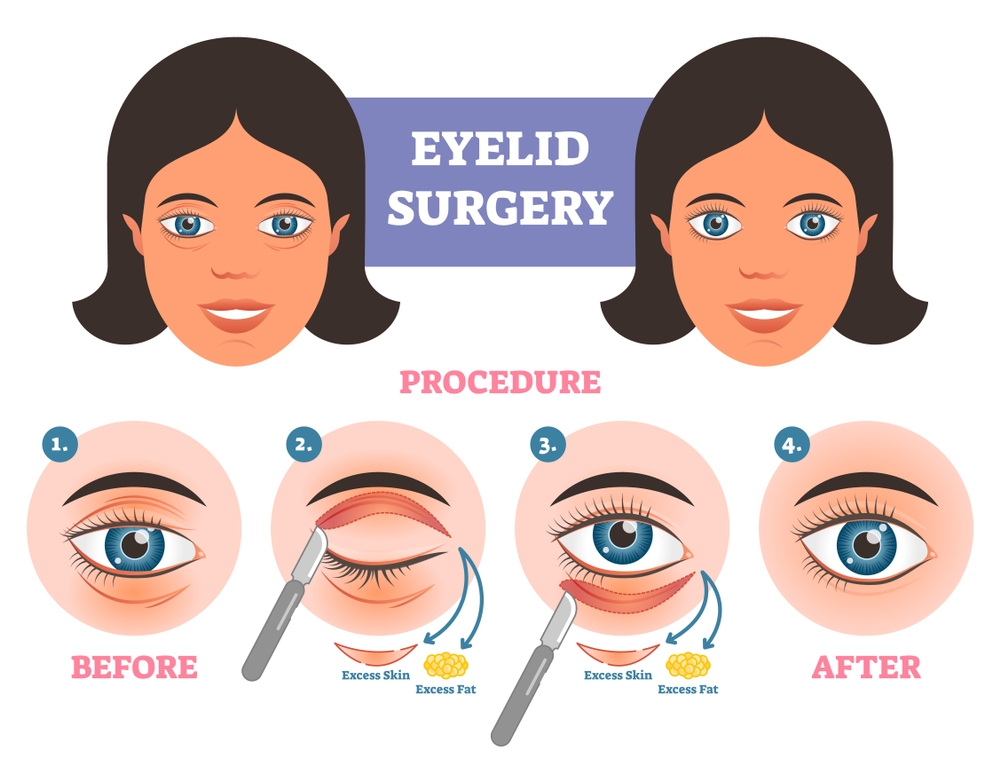
What is Oculoplasty?
Oculoplasty, also known as ophthalmic plastic surgery, is surgery with relation to the eye and its surrounding structures. Oculoplasty surgery may be performed to improve function, comfort and appearance for the following conditions:
- Tear Drainage Problems
- Eyelid Malposition
- Skin Cancers of the Eyelid
- Problems of the Orbit (eye socket)
- Eyebrow Problems
Who Needs an Ophthalmic Plastic Surgery?
Although your eye doctor is the best judge for suggesting you a surgery, the following are the symptoms which you may experience and know that you are in need of oculoplasty:
- Blinking of eyes more than necessary
- Eyelids Hanging Downwards (Ptosis)
- Twitching of eyes
- Wrinkles, scars or folds around the eyes
- Eyelids tearing in or out (Entropion/Ectropion)
- Blocked Tear Ducts (NLD Block)
- Tumors growing inside or surrounding the eye
- Blepharoplasty or excessive fat in eyelids
- Bulging Eyes
- The absence of an eye
- Orbit Tumors
- Burns of the eye
Ophthalmic Plastic Surgery at JAIBO Eye Centre in GWALIOR
The ophthalmologists at JAIBO are specially trained in the field of oculoplasty that essentially is a combination of ophthalmology and plastic surgery. There are various kinds of surgeries that are performed to take care of problems like NLD block, Ptosis, Entropion, and Ectropion, etc.
The oculoplasty treatment in GWALIOR starts with an examination of the current condition of the patients and what symptoms and problems they are having which are creating a hindrance either in their vision or their appearance.
Once the examination is done, the patients are suggested with the appropriate options of oculoplasty, and they are free to choose any of them. With state-of-the-art facilities, latest machines and up-to-date technology available with the oculoplasty surgeons at JAIBO Eye Centre, the surgery becomes a cakewalk for the patients. In some cases, the patients need to contact a neurosurgeon for an examination, which is communicated during the initial analysis of the patient’s condition.
All our surgeons take extra care while working with kids and teens since there are some eye muscles which are underdeveloped or which are quite week during the initial stages of growth.
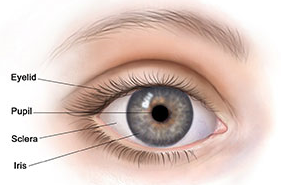
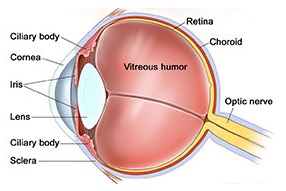
The eye is an important sense organ. It is made up of 3 coats. The outer coat is the cornea and sclera. The middle coat is the uveal tract and the inner coat is the retina. The uveal tract consists of 3 parts. The iris is the visible part of the uvea and gives color to the eye (blue, black, brown). The ciliary body is the middle layer of the uvea which manufactures the fluid inside the eye. The choroid is the posterior layer of the uvea which is rich in blood vessels.
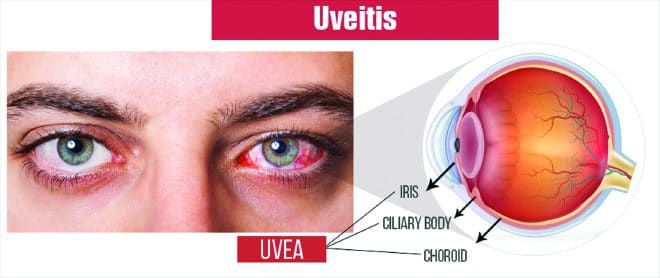
What is Uveitis?
Inflammation or swelling in any of the part of the uveal tract is called uveitis. Depending on the location of inflammation, it is called anterior uveitis (iris and ciliary body is involved), intermediate uveitis (ciliary body and the vitreous is involved), posterior uveitis (choroids and retina involved), panuveitisd (all layers of the uveal tract are involved).
What Causes Uveitis?
Causes of Uveitis are many.
- It may result from an infection (bacteria like tuberculosis, viruses like herpes, parasites like toxoplasmosis)
- It may also be related to an autoimmune disease (with or without involvement of other parts of the body). This essentially is when our immune system recognizes a part of our own body as foreign and elicits a reaction in the form of uveitis. The uveitis may be the presenting manifestation of an underlying systemic disease.
- It can occur as a result of injury to the eye.
- It can occur due to causes within the eye like cataract and retinal detachment
- Sometimes the cause is not known at the first instance. As we follow-up the patient over a period of time, we may be able to pick up new clues or signs suggestive of a systemic disease. In such cases, they are labeled as idiopathic (cause not known) at the initial visit.
What are the Symptoms of Uveitis?
Depending on the structure involved, the symptoms can vary from
- Pain
- Redness
- Inability to see light (photophobia)
- Black spots moving in front of the eye
- Blurring or reduction in vision
How is an Ophthalmic Evaluation Done in a Patient with Uveitis?
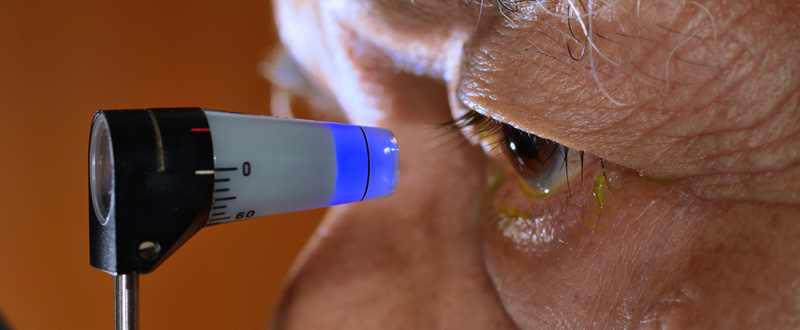
An initial examination of the eye will be done. This includes the recording of the visual acuity by reading a chart (to check if the vision has decreased), slit lamp examination; (in which a narrow beam of light is shone into the eye so that a magnifying lens can closely examine the highlighted portion of the eye). Intraocular pressure recording (a painless test done by a tonometer); fundus examination (in which the pupil is widened so that the ophthalmologist can look into the eye and see structures in the back of the eye).
Because uveitis can be caused by so many different things (infections/autoimmune diseases) diagnosis may require detailed laboratory investigations and a referral to a uveitis specialist.
What Does a Specialist Do?
A detailed medical history is elicited. As uveitis can occur due to infection or an underlying autoimmune disease, it is necessary to discover and treat these conditions as well. The results obtained in the routine laboratory tests and or imaging will be analyzed by the uveitis specialist. Many times a repeat in serologic testing may be needed. Specialized imaging of the eye and its structures may be required. Specialized blood tests related to the immune system may also be ordered to obtain a diagnosis. Depending on the type of uveitis, a sample of the fluid from the eye may also be sent to obtain a diagnosis by molecular diagnostic techniques. As uveitis may be related to a systemic disease, a cross consultation with a rheumatologist, a pulmonologist or a physician may also be done.
Why is Early Diagnosis of Uveitis Important?
Uveitis is the 3rd leading cause of blindness. Inflammation of the uvea can affect the cornea, retina, sclera and other vital parts of the body. Inflammation inside the eye is a medical emergency because, untreated, it will lead to vision loss. Damage to the eye is preventable if detected early and treated adequately.
How is Uveitis Treated?
The treatment of uveitis aims to achieve the following:
- Relief of pain and discomfort (when present)
- To prevent sight loss due to the disease or its complications
- To treat the cause of the disease where possible.
Medical treatment of uveitis must be aggressive to prevent glaucoma, to prevent scarring of the structures inside the eye and to prevent possible blindness.
Different medications are used to control the original cause of uveitis, if known and to minimize the inflammation itself. Eye drops especially steroids (to reduce inflammation and pain) and pupil dilators (to widen the pupil and relax the muscles within the eye) are the main medications used to treat uveitis. For deeper inflammations, oral medicines eye injections or intravenous injections of steroids may be necessary. More severe cases of uveitis and those intolerant to steroids may require treatment with immunosuppressive agents. Complications such as glaucoma, cataract or new blood vessel formation (neovascularisation) also may need treatment in the course of the disease. If complications are advanced, conventional surgery or laser surgery may be necessary.
What is the Expected Duration of Treatment?
The duration of treatment varies from person to person and also depends on the type and cause of uveitis. Simple forms of uveitis, for example, may respond to treatment within days and may not recur. Chronic (long term, recurring) forms of uveitis that threaten vision can be very difficult to cure and require persistence on the part of the treating physician(s) and patient. The length of time required to get the disease into a durable remission on steroids or immunosuppressants is difficult to quantify and is very individualistic but the minimum of 2 years is a reasonable estimate. With appropriate, targeted treatment, most people with uveitis will become well controlled and progress to emission. Once in remission from uveitis, you should expect to have regular follow-up visits to our doctor to make sure that the disease remains in remission.
You have to Help to Save Your Sight.
Find support and encouragement from your family, friends and others. Sometimes it helps to talk to people who have experienced the same thing. It can help you to discuss side effects, share ways to remember your medicines and celebrate getting your uveitis under control. Unfortunately, there are a few people who will lose vision despite commitment to working with their eye doctor and following their treatment plan.
The future holds great promise for uveitis. New medicines and treatments continue to be developed. In the meantime, take heart in knowing that we are doing everything possible to treat your condition. The doctor/patient team approach, support from others and promising scientific discoveries will help you look forward towards a bright future.
